 美ACOG今年5月更新的预防宫颈癌的宫颈涂片指南:
美ACOG今年5月更新的预防宫颈癌的宫颈涂片指南:从21岁开始,或性经历后3年开始;
21---29岁每三年一次;
30---65岁每5年一次宫颈涂片加HPV测试;
65岁以后属以下情况应停止筛查(无宫颈上皮异生史,过去10年连续三次涂片阴性)。
【Caption】 Hello. I'm Dr. Sandra Fryhofer. Welcome to Medicine Matters. The topic: Screening for cervical cancer. The American College of Obstetrics and Gynecology (ACOG) released new guidelines.[1]Here is why it matters.
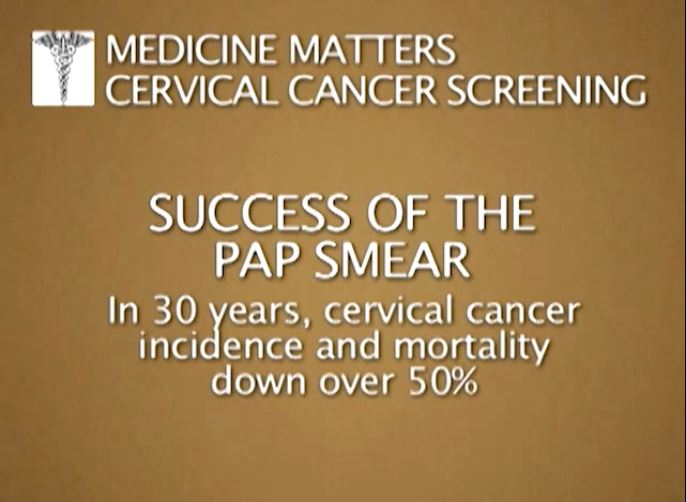
Kudos to the Pap smear. Over the past 30 years, incidence of mortality from cervical cancer in this country has dropped by more than 50%.[2] In fact, most cervical cancers occur in women who have either never been screened or who were not screened adequately. We have come a long way since 1928 when Dr. Papanicolaou first proposed cancer cells on a vaginal smear as an early warning. His landmark paper on this subject followed in 1941,[3] and the Pap smear has now evolved to liquid-based cytology.

Dr. George Papanicolaou, discoverer of the Pap Test Pap test abnormal.
Methodology for HPV DNA testing was FDA approved in 2000, and the first cervical cancer vaccine, the human papillomavirus (HPV) vaccine, hit the market in 2006. Still, American Cancer Society estimates of more than 12,000 new cases and more than 4000 deaths from cervical cancer in 2012 highlight the need for continued screening.[4]
As technologies have evolved, so have recommendations for screening. Many groups have gone on record with guidelines for cervical cancer screening, and now ACOG presents its new recommendations.[1]
The new guidelines take into consideration HPV and the natural history of cervical cancer. Most HPV infections are transient and the body is able to clear them. It is persistence in HPV infections that lead to cervical cancer. HPV is most common in teens and in women in their 20s. Most women, especially those under age 21, are able to clear the infection in 1-2 years. In women over 30, however, HPV infections are more likely to be persistent and rates of high-grade lesions are increased. Most HPV-related lesions progress to cervical cancer slowly. It takes, on average, 3-7 years for severe dysplasia to progress to invasive cervical cancer. With that as a background, here are the details.
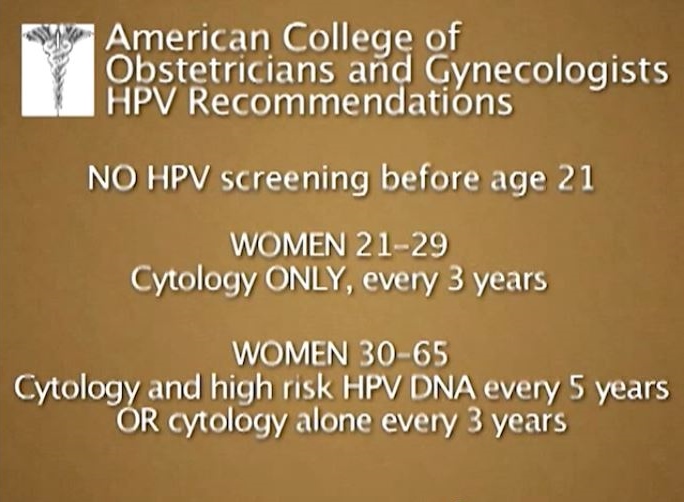
First, when to start screening. Don't start testing until age 21, regardless of behavior, risk factors, and age at first sex.
-
For women aged 21-29, cytology screen only every 3 years and do not conduct HPV testing.
-
Starting at 30 and through age 65, co-test every 5 years with both cytology and HPV testing. A high-risk HPV DNA test is the preferred recommendation, but cytology alone every 3 years is also acceptable. HPV testing alone is not.
-
After age 65, future screening recommendations depend on past screening results. If previous tests have been negative, these women get a pass. No more screenings needed. Negative [in this case] means 3 consecutive negative cytology results or 2 consecutive co-testing results in the past 5 years.
-
Women with a history of CIN2, -3, or adenocarcinoma can't stop [screening] at age 65. They must continue screening.
What about after hysterectomy? Do you still need testing? If the cervix is removed and there is no history of CIN2 or higher, the woman is done. No more screening is needed. But for those with high-grade lesions before hysterectomy, keep screening with cytology every 3 years for the next 20 years. That is because recurrent cancer can develop at the vaginal cuff even years later. The role of HPV testing in this setting is unclear.
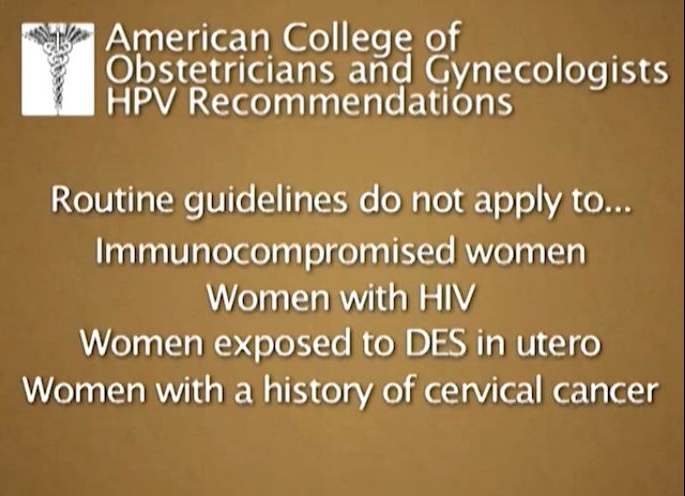
These are routine guidelines and don't apply to women who are immunocompromised, HIV positive, were exposed to diethylstilbestrol (DES) in utero, or with a history of cervical cancer.
Cervical cancer screening: It is a gold-standard example of how screening has saved lives. Thank you, Dr. Papanicolaou. For Medicine Matters, I'm Dr. Sandra Fryhofer.
复习一下视频里的几张重要截图:





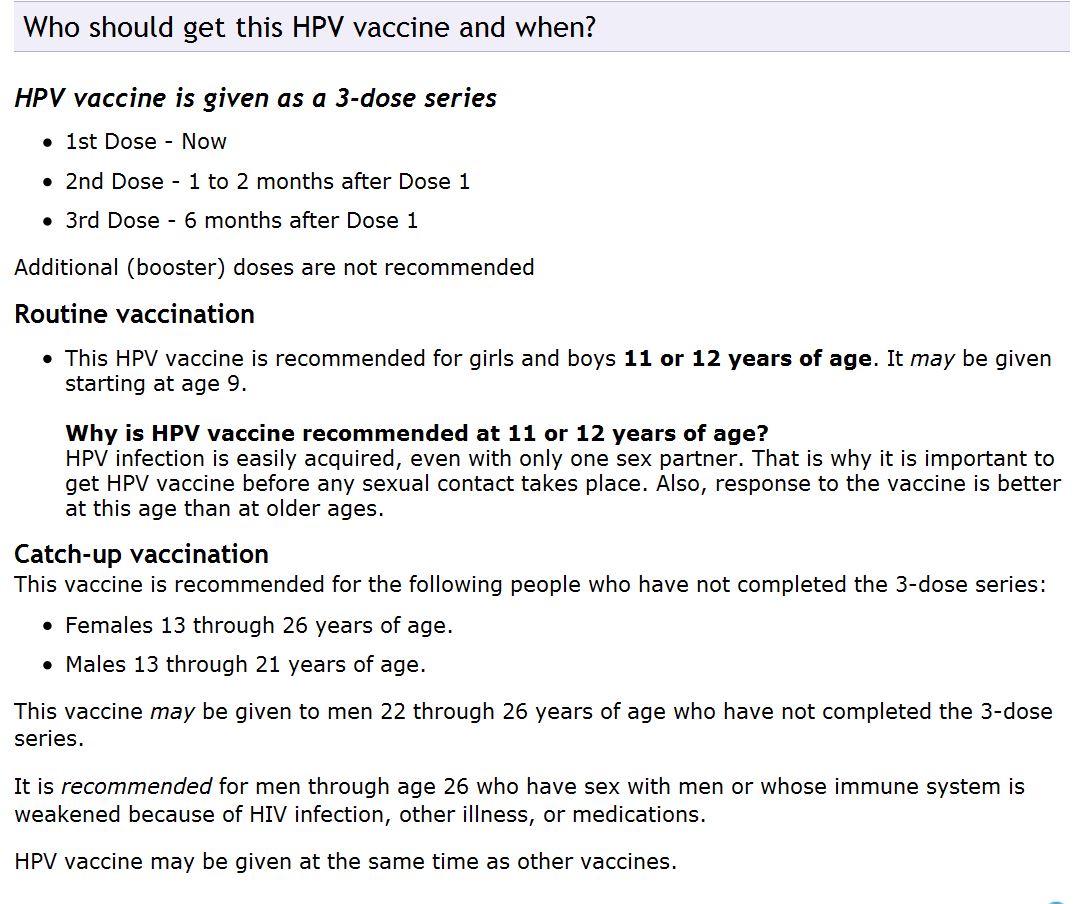
- HPV (Human Papillomavirus) Gardasil® VIS Current Edition Date: 5/17/2013. ... HPV (Human Papillomavirus) Gardasil® Vaccine. ...
References
-
American Congress of Obstetricians and Gynecologists. ACOG practice bulletin no. 131: screening for cervical cancer. Obstet Gynecol 2012;120:1222–38. http://www.acog.org/About%20ACOG/Announcements/New%20Cervical%20Cancer%20Screening%20Recommendations.aspx Accessed May 22, 2013.
-
Vesco KK, Whitlock EP, Eder M, Burda BU, Senger CA, Lutz K. Risk factors and other epidemiologic considerations for cervical cancer screening: a narrative review for the U.S. Preventive Services Task Force. Ann Intern Med. 2011;155:698-705. http://www.uspreventiveservicestaskforce.org/uspstf11/cervcancer/cervcancerart.htm Accessed May 22, 2013.
-
Papanicolaou GN, Traut H. The diagnostic value of vaginal smears in carcinoma of the uterus. Am J Obstet Gynecol (St. Louis). 1941;42:193-206.
-
American Cancer Society. What are the key statistics about cervical cancer? 2013. http://www.cancer.org/cancer/cervicalcancer/detailedguide/cervical-cancer-key-statistics Accessed May 22, 2013.