Image copyright Thinkstock
Image copyright Thinkstock
研究发现:“好”胆固醇不总是都好 (ZT)
研究发现:“好”胆固醇不总是都好
转自BBC:
http://www.bbc.com/zhongwen/simp/science/2016/03/160311_good_cholesterol_not_always_good
 Image copyright Thinkstock
Image copyright Thinkstock
(吃与活注:viewfinder发现图标的说法有误,橄榄油,坚果,牛油果等植物中并没有胆固醇)
一项研究发现,一些人的“好”胆固醇水平高,可能患心脏病的风险更高。
人们通常把胆固醇分为好胆固醇与坏胆固醇,好胆固醇是指高密度胆固醇(HDL),坏胆固醇则指低密度胆固醇(LDL)。
通常来说,坏胆固醇是在血管壁上的脂肪沉淀物。这种胆固醇过高可能堵塞血管,容易引发心脑血管疾病;而好胆固醇就像清道夫一样可以带走人体中血管中的坏胆固醇,把它交给肝脏处理,排出体外。
但是英国剑桥大学的研究人员发现,太多的好胆固醇并非总是好事。
有些食品,例如橄榄油、鱼和坚果富含好胆固醇。医生在测试病人有多大几率犯心脏病的时候,会考虑好胆固醇的含量。
然而,研究人员发现,由于罕见的基因突变,可能会使好胆固醇水平高的人患心脏病的风险增加80%,相当于吸烟者的风险。
这种基因叫做SCARB1,影响一小部分的人,大约比例为1:1700,即每1700人当中有1人会受到影响。
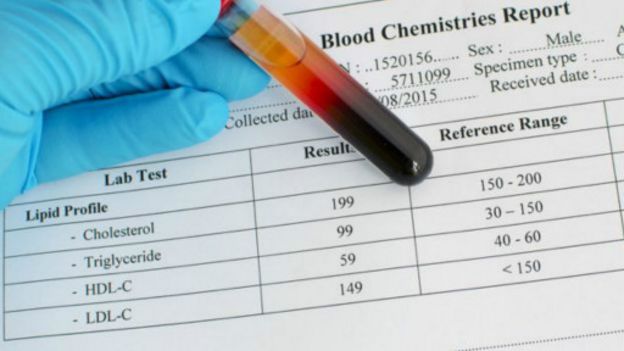 Image copyright Thinkstock
Image copyright Thinkstock
试验显示,正是由于发生了基因的突变,使得好胆固醇无法把收集的坏胆固醇交给肝脏处理,从而给人体带来更大的隐患。
这一发现之所以非常重要是因为以前人们没有想到好胆固醇也可能对人体有害, 特别是一些提升人体好胆固醇的药物。
这也是首次研究显示,一些体内好胆固醇水平高的人可能面临更大的心脏病风险。
同时,该试验也显示投入大量精力研制的提高人体内好胆固醇水平的药可能没有什么用。
剑桥大学的巴特沃思教授说,好胆固醇颗粒的大小,以及他们运输坏胆固醇的能力等可能更重要。
同时,研究人员说,运动既可以提高人体内的好胆固醇,也可以降低心脏病的危险。
(编译:凯露 责编:高毅)
原始文献:
英文介绍:
Penn Study Shows a Form of Genetically Elevated "Good" Cholesterol May Actually be Bad
Research has implications for better understanding the relationship between "good" cholesterol function – in addition to level -- and heart disease risk
PHILADELPHIA – The generally accepted medical maxim that elevated HDL cholesterol (HDL-C) is “good” has been overturned by a multi-center, international study, led by researchers from the Perelman School of Medicine at the University of Pennsylvania. They show that a certain genetic cause of increased HDL-C may actually be “bad,” noting that a specific mutation in a gene which encodes a cell receptor protein that binds to HDL prevents the receptor from functioning. The mutation causes an increased risk of coronary heart disease even in the presence of elevated levels of HDL-C or “good” cholesterol. Their findings are published this week in Science.
Rader and his colleagues sequenced the lipid-modifying regions of the genomes of 328 people with markedly elevated HDL (along with a control group with lower HDL) to identify genetic causes of high HDL. One of the genes they focused on was SCARB1, which encodes for Scavenger Receptor B1 (SR-B1), the major receptor for HDL on cell surfaces.
In the course of this sequencing, they identified, for the first time, a person without any SCARB1 function, typified by an extremely high HDL-C level of about 150 mg/dL, whereas the normal level is about 50 mg/dL. The subject had two copies of a SCARB1 mutation called P376L, which the team showed caused a breakdown in HDL receptor function.
Among the many approaches they took, the researchers generated induced pluripotent stem cells (iPSCs) from the SCARB1-deficient person, used them to create liver cells, and showed these new cells had profound reduction in their ability to take up HDL. “This mutation prevents the receptor from getting to the cell surface where it needs to be situated in order to bind and take up HDL,” Rader explained. “This disruption in the receptor’s job is due to mistakes in its folding and processing during protein synthesis.”
Going back to the other sequenced genomes, the researchers were then able to show that persons who carry only one copy of the SCARB1 P376L mutation have significantly higher HDL-C levels. From this, Rader and colleagues had a hunch, based on their knowledge of SCARB1 function and previous studies in mice, that having the SCARB1 P376L mutation, despite raising HDL, might paradoxically increase the risk of heart disease.
Working with other researchers around the world, the Penn team was able to show exactly what they had surmised. “This SCARB1 variant, while rare, is just frequent enough that it allowed us to ask the question about its effect on HDL and heart disease in people with only one copy of the mutation," Rader said.
The Penn team and their colleagues plan to characterize and test other SCARB1 mutations for their relationship to HDL levels and heart disease. Other genes may also have similar effects. “Eventually we may want to perform genetic testing in persons with high HDL to make sure they don't have mutations--like this one--that raise HDL but don't protect against, or may even increase, risk for heart disease,” Rader said. Since the P376L mutation in SCARB1 appears to be specific to people of Ashkenazi Jewish descent, testing in this ethnic group might be particularly important.
Rader suggests that a therapeutic approach to increase the expression or activity of SCARB1 could be a new way to reduce the risk of heart disease even though it would reduce HDL blood levels. “The work demonstrates that the protective effects of HDL are more dependent upon how it functions than merely how much of it is present,” Rader concluded. “We still have a lot to learn about the relationship between HDL function and heart disease risk.”
This work was led by three co-first authors in the Rader lab, postdoctoral fellow Paulo Zanoni, MD/PhD student Sumeet Khetarpal, and medical student Dan Larach.
This work was supported in part by the National Center for Research Resources (TL1RR024133), the National Center for Advancing Translational Sciences (TL1R000138), and the Doris Duke Charitable Foundation.